
Asthma and Pregnancy - What You Need to Know - Ashcroft Pharmacy
Asthma and Pregnancy: Understanding the Risks
Managing your health conditions during pregnancy is vital for your well-being and your baby's. If asthma isn't controlled, complications can arise for both of you. Problems like low birth weight and premature delivery are more likely if asthma isn't managed properly during pregnancy.
When asthma isn't well-controlled, your blood may have less oxygen. This affects your baby, too, as they need oxygen from your blood. Insufficient oxygen could impact your baby's growth and health. Managing asthma is safer for your baby than not treating it. With proper asthma control, you can expect a normal pregnancy.
Other observed patterns include:
- Improved asthma gradually progresses during pregnancy.
- Asthma is generally milder in the last pregnancy month.
- Worsened symptoms often appear between weeks 29 and 36.
- Labor and delivery usually do not worsen asthma.
- First pregnancy's symptoms often mirror later pregnancies.
Risk factors for attacks — what increases or decreases attack risk during pregnancy is not fully clear. Modifiable risk factors like smoking, being overweight, depression or anxiety, uncontrolled asthma, and poor medication adherence heighten attack risk.
Chances of asthma attacks during pregnancy are not constant; they are highest between weeks 17 and 24. Some women mistakenly stop taking asthma medications when they find out they're pregnant, which raises the risk of attacks.
Asthma severity During Pregnancy
For an Asthma Patient, it is tough to predict how your asthma symptoms will change during pregnancy. They might improve, stay the same, or even worsen.
Asthma's severity during pregnancy varies from woman to woman. It is tough to predict how asthma will behave in a woman's first pregnancy. Older info said asthma worsened in one-third, improved in one-third, and stayed the same in one-third. Recent info suggests 18.8 % may have worse asthma control during pregnancy, while others stay the same.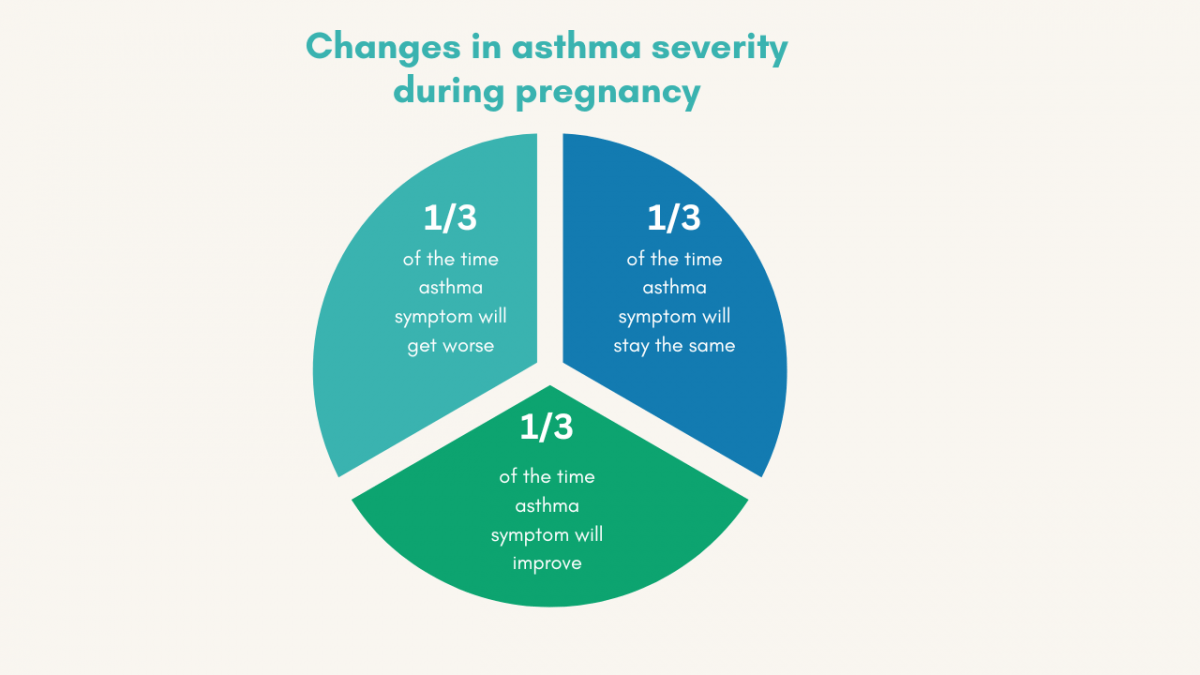
- About one-third of pregnant people with asthma might feel worse.
- Another one-third might not see any change in their asthma symptoms.
- The last one-third might feel better with their asthma during pregnancy.
Getting Back to Normal:
- If your asthma symptoms change while you're pregnant, most of the time they go back to how they were within three months after you've given birth.
Pregnancy Predictions: If your asthma behaves differently in one pregnancy, it might do the same in your future pregnancies, but it is hard to be sure.
Collaborate with Doctors:
If you have asthma and plan to become pregnant, discuss your condition with a doctor. Because it's not easy to predict, it's really important to work closely with your doctors.
This means teaming up with your pregnancy doctor, your regular doctor, and the doctor who knows about your asthma. They will keep an eye on your asthma and change your treatment if needed to keep you healthy. It's like a team effort.
Asthma Effects on Pregnancy & Baby
If your asthma is well controlled, there is no significant risk to you or your unborn child. It is important to note that uncontrolled asthma can lead to serious complications, though the reasons behind these remain unclear. In comparison to those without asthma, individuals with asthma have a slightly elevated likelihood of encountering the following pregnancy complexities:
- Opting for a cesarean delivery
- High blood pressure or preeclampsia
- Giving birth prematurely
- Delivering a baby smaller than typical for their gestational age
- It’s important to emphasize that majority of pregnant individuals with asthma, as well as their babies, navigate pregnancy without any complications. Effective asthma management during pregnancy significantly reduces the risk of these complications.
How to control asthma during pregnancy
Asthma symptoms might change during pregnancy—improve, remain stable, or worsen. In fact, around 45% of pregnant women with asthma experience an asthma attack while pregnant. For effective asthma management during pregnancy, your healthcare team collaborates with you to:
Handling Your Asthma While Pregnant
Keep Your Asthma Well-Controlled
Uncontrolled asthma can lower oxygen levels for your baby. Minimize asthma triggers like dust mites and secondhand smoke. Consider flu and COVID-19 shots (safe for pregnancy) to lower the risk of severe infections.
Certain asthma medicines might be safer during pregnancy, so your treatment plan might change. Collaborate with your doctors to find the most suitable treatment for you. You can take steps to manage your asthma during pregnancy:.png)
- Keep up with exercise and a healthy diet.
- Control hay fever with safe antihistamines—check with a doctor or pharmacist.
- Quit smoking, and tips on stopping smoking in pregnancy.
- Control both daytime and nighttime asthma symptoms.
- Maintain lung function and normal activity levels.
- Avoid things that trigger your allergies, like pet fur.
- Avoid hay fever triggers, like mowing the lawn.
- Get the flu jab while pregnant.
- If you get a cough or cold, use a preventer inhaler (steroids) and consult a doctor about this during pregnancy.
Take Asthma Madication
There are plenty of asthma medications that are safe during pregnancy, so it's a good idea to chat with your asthma doctor about your options. If you have been using asthma medication before pregnancy, don't stop without having a talk with your doctor first.
When it's time to have your baby, having asthma medication available is important. Discussing this ahead of time with your healthcare team will let them include it in your birthing plan. To keep asthma in check during pregnancy, it is important for expectant moms to keep an eye on their symptoms.
Stay away from asthma triggers, and take the prescribed asthma medicines. Stopping your asthma medicines suddenly could be risky for both you and your baby. Make sure to keep up with appointments with your asthma care provider throughout your pregnancy and don't forget to get your annual flu shot --it is safe for pregnant women.
Monitoring
Lung Checkup: Monitoring your lung function is crucial. Tests at the doctor's office can help measure how well your lungs are working.
Home Help: Using a peak flow meter, a simple device, can show if your airways are narrowing. If the reading drops, your asthma might need more attention.
Regular check up for Baby's Health During Pregnancy:
Doctors keep an eye on how the baby is doing during regular checkups throughout pregnancy. Especially if you have asthma symptoms or an asthma attack. You should also pay attention to your baby's movements. If you notice your baby isn't moving as usual, talk to your pregnancy doctor right away.
Two ways they might monitor the baby's well-being:
- Non-Stress Testing: Sometimes, after 32 weeks of pregnancy, if you often have asthma symptoms or attacks, they might suggest a non-stress test. This test checks on the baby's condition.
- It's done by putting a small ultrasound device on your belly to check up the baby's heart rate. The baby's heart rate should go up When your baby moves. They look for at least two increases in the baby's heart rate within 20 minutes. If these increases don't happen after 40 minutes of monitoring, more tests might be needed.
Ultrasound Check: Sometimes, they use ultrasound to see how the baby is growing and moving how much fluid is around the baby. Keeping an eye on the baby's health helps make sure everything is going well for both of you.
Labor and Delivery
Discuss with your healthcare team about your labor and delivery plan. If you have asthma, they'll pick safe medicines for you and your baby. For instance, during an emergency C-section, they might choose anesthesia that helps open your airways.
Belly breathing exercises are useful during labor. The Lung Association has a video to help you practice. This skill is handy for those with asthma during pregnancy or whenever you might have trouble breathing.
Education
Understanding Asthma: Learning about asthma empowers you to manage it better. Recognize signs, avoid triggers, and use medications correctly. This knowledge is especially important during pregnancy.
Asthma Medication During Pregnancy
If you're pregnant and have asthma, don't worry about using your asthma medications. Your allergist will guide you in choosing safe options during pregnancy.
Asthma symptoms can vary during pregnancy, so creating a plan with your allergist is important. The plan should be based on the severity of your asthma and your history with asthma medications while pregnant. Remember, medication should not replace avoiding triggers – staying away from irritants can reduce your need for medication.
Inhaled Medicines: Albuterol (Ventolin Inhaler) is the most commonly prescribed inhaled medication. These are often preferred as they have a precise effect and only a small amount enters your bloodstream. However there are concerns about whether Albuterol is safe or not during pregnancy. .png)
Proven Medicines: Older medicines with a good track record during pregnancy are usually preferred.
- First Trimester: It's best to use fewer medicines during the first 3 months when the baby is developing. But don't worry, birth defects from meds are really rare – only around 1% of all birth defects come from medicines.
- Continued Use: Usually, the same medicines that are safe during pregnancy can also be used during labor and delivery.
Thankfully, most asthma patients do well during labor and delivery, with close baby monitoring. For low-risk women with well-controlled asthma, regular baby monitoring is enough. Women with severe asthma or other risks might need to be more careful observation.
The main goal is to keep your asthma under control throughout pregnancy. To do this, stick to your treatment plan and take your meds as instructed.
- Rarely need your reliever inhaler (rescue inhaler).
- Sleep well without asthma symptoms.
- Pregnancy doesn't change asthma treatment goals. Controlled asthma means you:
- Experience minimal or no daytime symptoms.
- Carry out everyday activities normally.
- Maintain normal or near-normal lung function.
Using asthma medications is safer for you and your baby than risking an asthma episode.
Warning:
Don't quit your asthma medicine without talking to a doctor or asthma specialist. Most asthma meds are safe while pregnant. If your asthma is under control, there is not much risk for you or your baby. Keep taking your prescribed asthma meds during pregnancy, unless your asthma gets worse. Stopping meds could make your symptoms worse and harm your health.
Study
A recent study shows that 18.8% of pregnant women experienced worsened asthma symptoms, which is lower than previous data. This worsening was notably linked to the severity of the disease. Challenges also arise in managing asthma during pregnancy. Studies indicate that about 65% of patients struggle to control their asthma while pregnant. Moreover, 64.4% have incorrect inhaler technique, only 38% can differentiate between asthma medications – relievers and controllers, 12.7% receive a written asthma action plan, 17% undergo spirometry in the past 5 years, and 3.8% have a peak expiratory flow meter at home.
Bottom Line
However, for successful asthma management during pregnancy, regular medical care and adherence to the treatment plan are key. If you are pregnant, it is advised to have a conversation with your healthcare provider about the suitable asthma medication for you.
FAQ
Can I have to stop asthma medication during pregnancy?
If you discover you are pregnant, do not have to stop your asthma medications. Doing so could be risky for both you and your baby. So don’t stop your asthma medicine during pregnancy . It's safe during pregnancy and important for you and your baby. If you're worried or want to make changes, talk to a doctor first.
What If My Asthma Isn't Well-Controlled During Pregnancy?
When your asthma isn't properly managed, your blood's oxygen levels might drop, affecting your baby's oxygen supply too. Keeping your asthma well-controlled also reduces the likelihood of pregnancy problems like premature birth, low birth weight, and preeclampsia (high blood pressure during pregnancy).
Is It Safe to Use My Inhaler During Pregnancy?
Using your inhaler is safe. Short-acting medications found in inhalers, such as albuterol, levalbuterol, pirbuterol, and ipratropium, pose no harm to both you and your baby. Treating your asthma with inhalers not only reduces the risk of attacks but also improves your lung function.
How Can I Make Asthma Less Harmful for My Baby?
To help keep your baby safe during your pregnancy:
1. Work with your asthma doctor: They'll guide you on the right medication and dosage.
2. Know your triggers: Keep a record of what worsens your asthma and try to avoid those things.
3. Get coordinated care: Make sure your asthma doctor and pregnancy provider work together for your well-being and your baby's health.
Can Pregnancy Make Asthma Worse?
Wondering if pregnancy could affect your asthma? Well, it's a bit of a mixed bag. Your asthma might stay the same, get a tad worse, or surprisingly, even improve. Usually, if your asthma is already quite severe, it could act up a little during pregnancy. On the flip side, if your asthma behaved itself in a previous pregnancy, chances are it'll behave the same way next time.
Don't worry, having asthma usually shouldn't stop you from getting pregnant. But if your asthma is pretty intense, have a chat with your doctor before you start trying. And if your asthma is linked to allergies, try your best to avoid those triggers. That might mean staying away from things like pet dander, dust mites, cockroaches, pollen, and indoor mold.
Can Asthma Attacks Happen During Labor?
When your asthma is under control, asthma attacks rarely occur during labor and delivery. Moreover, most individuals with well-managed asthma can perform breathing techniques during their labor without encountering difficulties.
Is Breastfeeding Safe?
Doctors generally consider asthma medicines safe for nursing babies when taken in regular doses. However, the extent of asthma medicine transfer into breast milk hasn't been extensively studied. While breastfeeding, it's crucial to stay hydrated by drinking enough fluids, which is important for everyone with asthma.
Can My Baby Get Asthma?
The chances depend on genes. If your family has asthma, your baby could too. Plus, the environment matters too.
Can I Stop My Baby from Getting Asthma?
Stopping smoking matters a lot because it's a big prenatal risk. Other things count too, like:
- How stressed you are during pregnancy.
- What you eat.
- Your vitamin D levels.
- When antibiotics are used.
- How your baby is delivered.
Discuss with your doctors to figure out your risks and make safe changes before your baby is born.
Sourses: NCBI, aafa.org, NHS.UK, lung.org, breathe.ersjournals.com




